Vitalant offers three health plan options through Aetna and Kaiser. Log into kp.org to locate a Kaiser provider or log into aetna.com to locate an Aetna provider.
The table below summarizes the key features of the health plans. The coinsurance amounts listed reflect the amount you pay. Please refer to the official plan documents for additional information on coverage and exclusions.
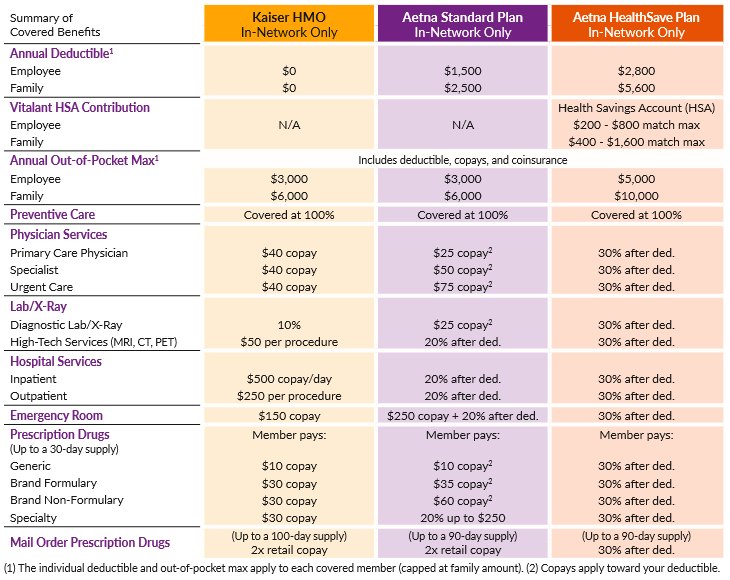
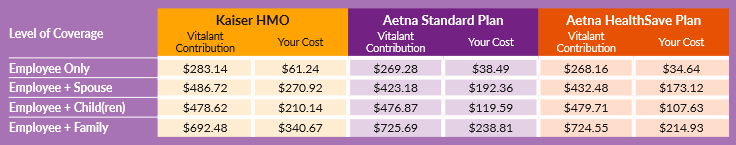
HEALTH INSURANCE COSTS
Listed below are the biweekly (24 pay periods) costs for health insurance. The amount you pay for coverage is deducted from your paycheck on a pre-tax basis.
In-network preventive care is free for health plan members.
The Vitalant health plans pay 100% of the cost of preventive care when received from a network provider. This means you won’t have to pay anything out of your pocket.
What Is Preventative Care?
The focus of preventive health care is to PREVENT illnesses, disease, and other health problems, and to DETECT issues at an early stage when treatment is likely to work best.
Why Is Preventative Care Important?
It is important that you have a preventive exam each year—even if you feel healthy and are symptom free—in order to IDENTIFY FUTURE HEALTH RISKS.
What's Covered?
Covered preventive services VARY BY AGE AND GENDER. Talk with your provider to determine which screenings, tests, and vaccines will be covered, when you should get them, and how often.
TELADOC
Aetna health plan members have 24/7/365 access to licensed physicians through Teladoc. This program saves you time and money by allowing you to seek information, advice, and treatment without having to face waiting lines at your doctor’s office or an urgent care center. In many cases you can even request prescriptions or refills without an office visit.
Use Teladoc when:
- Your primary physician is unavailable.
- You need treatment after normal business hours.
- You are traveling and need medical advice.
- You need help with non-emergent medical issues.
DERMATOLOGY CARE
Teladoc makes skin care easier. You no longer have to wait weeks for an appointment. Use your Teladoc account to upload images of your skin condition. U.S. board-certified dermatologists will give you a diagnosis and treatment plan customized to fit your specific needs within two business days or less.
The Teladoc dermatologists diagnose skin issues and treat common conditions like acne, psoriasis, eczema, rosacea, rash, poison ivy, skin infections, and dermatitis.
You will pay $75 per visit (until your deductible is met, then subject to coinsurance).
THERAPY
Teladoc provides treatment for the whole person, body, and mind. Speak with a licensed counselor, therapist, or psychiatrist by secure video visits seven days a week. You can find support for anxiety, relationship and family problems, emotional difficulties, work pressures, grieving issues, and trauma resolution.
You will pay a $160 fee for your first visit and $80–$90 per visit for follow ups (until your deductible is met, then subject to coinsurance).
GET STARTED
Connect with a licensed provider by calling 800-835-2362 (800-TELADOC) or by going online to teladoc.com/aetna. To get started, you must complete your medical history online or by phone prior to requesting a consultation.
KEY TERMS TO KNOW
Copay
A fixed dollar amount that you may pay for certain covered services. Typically, your copay is due up front at the time of service.
Deductible
The amount that you must pay each year for certain covered health services before the insurance plan will begin to pay.
Coinsurance
After you meet your deductible, you may pay coinsurance, which is your share of the costs of a covered service.
Out-of-Pocket Maximum
This includes copays, deductibles, and coinsurance. Once you meet this amount, the plan will pay 100% of covered services the rest of the year.
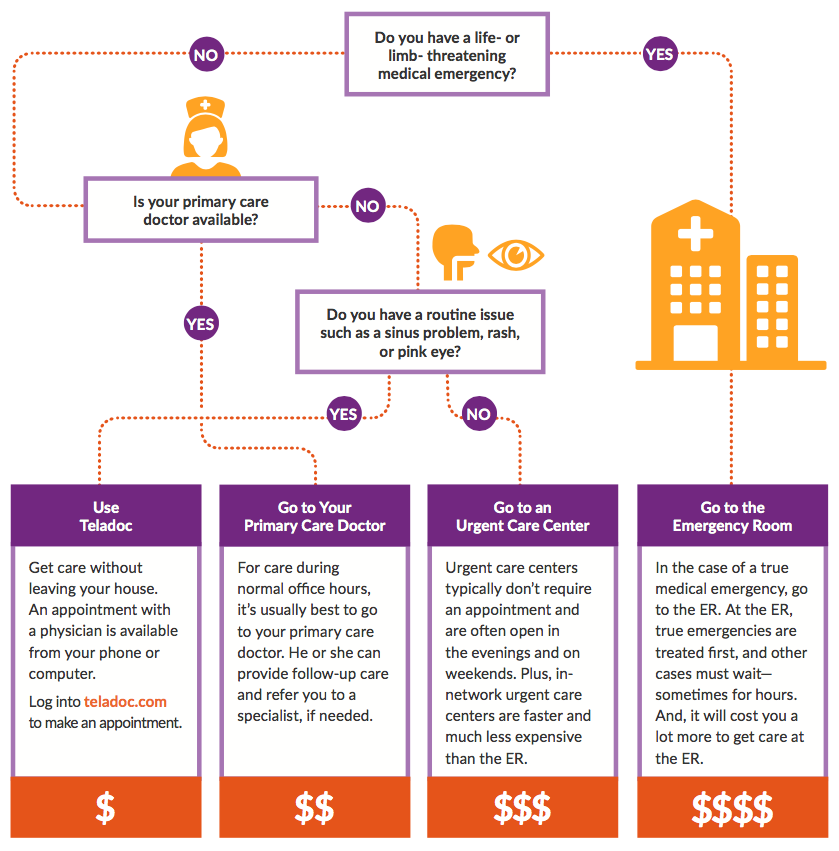
Know where to go for your health care.
Where you go for medical services can make a big difference in how much you pay and how long you wait to see a health care provider. Use the chart below to help you choose where to go for care.
AETNA TOOLS AND RESOURCES
Aetna health plan members have access to the following tools and resources to help enhance overall health and wellbeing. For more details about the Aetna health plans, visit aetnaresource.com/vitalant.
AETNA.COM
Aetna.com is your online resource for personalized benefits and health information.
When you register at aetna.com, you can access the following information on any device:
- In-network providers and facilities.
- Benefits and claims status.
- Cost estimates for prescriptions and care.
Visit aetna.com and log into your member website.
STEPS TO A HEALTHIER LIFE
This free, online health coaching program lets you choose an area of your health to focus on. And you set the pace, so you can accomplish your health goals in your own time.
- Each program is divided into small steps, so you can benchmark your progress along the way.
- Smart, interactive, and fun—Aetna’s online health coaching programs will provide you with strategies for success and support to meet your goals.
PRESCRIPTION DRUG COVERAGE
AETNA STANDARD FORMULARY
The Open Access Aetna Select health plan utilizes the Aetna Standard Formulary. A formulary is a list of drugs covered under your plan, with details about the type of coverage. There are certain medications that are not covered under your plan. Log into aetna.com to review the Aetna Standard Formulary.
MAINTENANCE CHOICE
After two retail fills of a maintenance medication, you will be required to fill a 90-day supply of your maintenance drug through Aetna Rx Home Delivery or at a CVS Pharmacy. Your doctor will need to write your prescription for a 90-day supply. Call the toll-free number on your Aetna member ID card for help getting started with 90-day supplies
ENHANCED CLINICAL REVIEW
Medical tests and procedures typically require prior approval before they can be performed. Aetna’s enhanced clinical review program uses medical specialists and diagnostic tools to review the doctor’s request.
An efficient process delivers the approval in four steps:
- Prescribe: Your doctor orders a test or procedure to diagnose or treat your condition.
- Submit: The doctor’s office submits the request for clinical review.
- Review: Aetna uses a separate independent company, eviCore, to perform the review. eviCore reviews the request using national medical standards, applying the expertise of clinical experts and considering the doctor’s area of expertise. The goal is for you to get the highest medical quality with the lowest out-of-pocket expense.
- Approve: In most cases, the request is approved in a few minutes or less. In some cases, a discussion between doctors is necessary for further clarification.
What tests and procedures are reviewed?
The program covers high-tech radiology (including: nuclear cardiology, MRI/MRA, PET scan, stress echocardiography, diagnostic right and left heart catheterization), diagnostic cardiology, sleep studies management, cardiac rhythm implant devices, and radiation oncology therapy.
What if a request is denied?
In some cases, an alternative recommendation is indicated during the review process.
What happens after a denial?
If there is a denial, your physician can discuss the case with an eviCore medical director to determine the best course of action. Often, additional medical information is all that is needed.
What happens if my doctor forgets to submit a request for clinical review?
Your doctor will need to submit a request within 14 business days of the date of service. All authorizations that are requested beyond the 14 business days will be denied.
