Medical
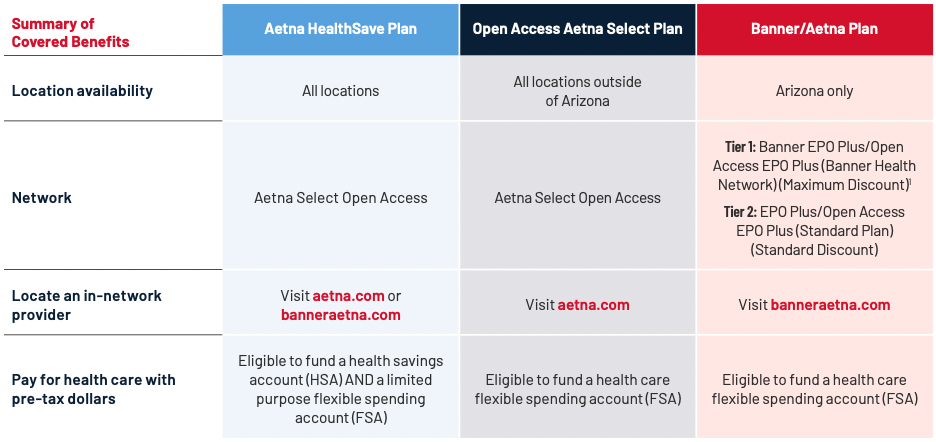
Grifols offers comprehensive medical insurance. The medical plans that you are eligible for depend on your location.
The plans provide in-network benefits only. Services received by non-network providers will not be covered by the plans. The table below highlights key features of the medical plan options.
(1) The Tier 1: Banner Health Network - Banner EPO Plus/Open Access EPO Plus is only available to those who live in Arizona. If you are traveling outside these areas or you have a dependent who lives outside these areas, you would access the Tier 2: EPO Plus/Open Access EPO Plus (Standard Plan) which is a national network.
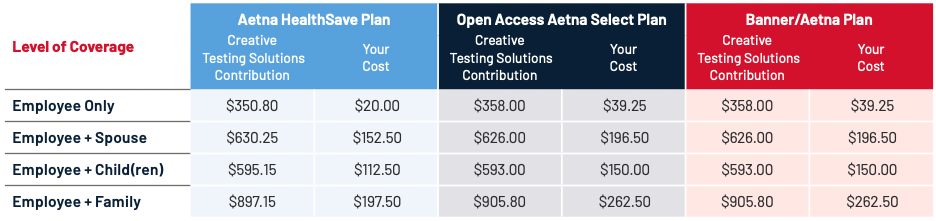
Medical Insurance Costs
Listed below are the biweekly (24 pay periods) costs for medical insurance. The amount you pay for coverage is deducted from your paycheck on a pre-tax basis, which means you don’t pay taxes on the amount you pay for coverage.
Spousal Surcharge
A working spouse surcharge of $200 per month ($100 per pay period) applies if your spouse is offered medical insurance through his or her employer and enrolls in a Grifols medical plan.
The table below summarizes the benefits of the medical plans.
The coinsurance amounts listed reflect the amount you pay. Please refer to the official plan documents for additional information on coverage and exclusions.
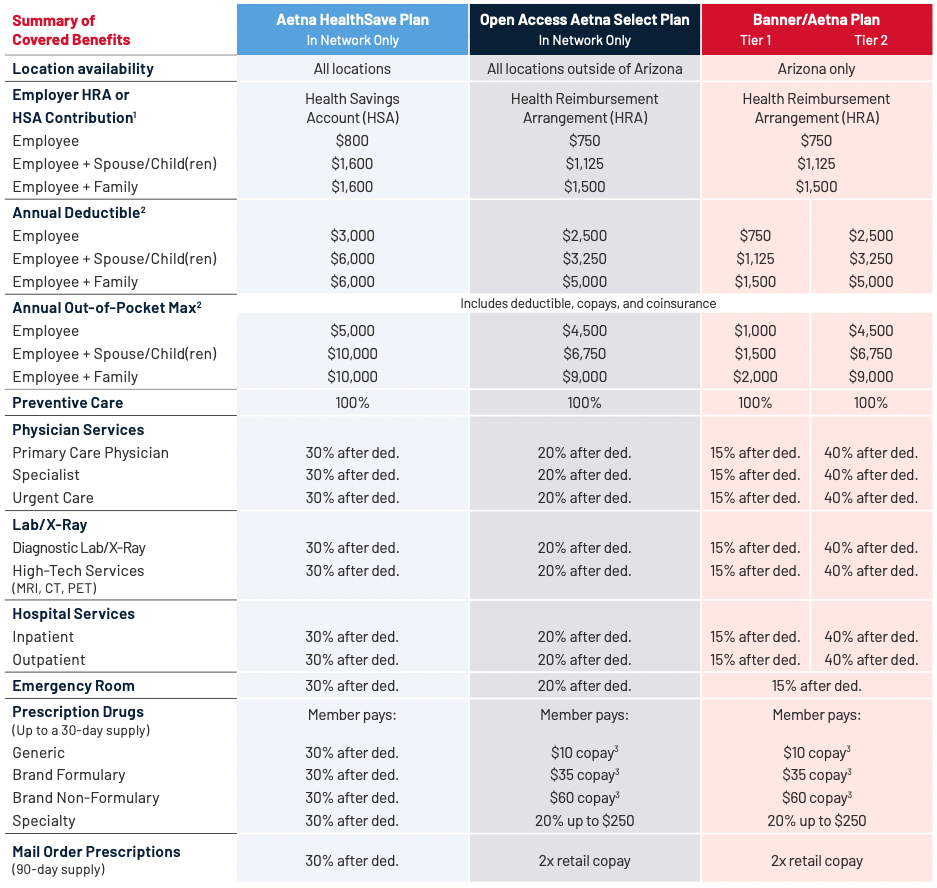
(1) The HealthFund contribution applies toward your deductible. The amount is prorated based on your date of hire. (2) The individual deductible and out-of-pocket max apply to each covered member (capped at family amount).
(3) Copays apply toward your out-of-pocket maximum. They do not apply toward your deductible.
Preventive Care
In-network preventive care is 100% free for medical plan members.
You won’t have to pay anything out of your pocket when you receive in-network preventive care. Practice preventive care and reap the rewards of a healthier future.
Preventive care helps keep you healthier long-term.
An annual preventive exam can help IDENTIFY FUTURE HEALTH RISKS and treat issues early when care is more manageable and potentially more effective.
Preventive care helps keep your costs low.
With a preventive care exam each year, you can TARGET HEALTH ISSUES EARLY when they are less expensive to treat. You can also effectively manage chronic conditions for better long-term health.
Preventive care keeps your health up to date.
Yearly check-ins with your doctor keeps your health on track with AGE- AND GENDER-SPECIFIC EXAMS, VACCINATIONS, AND SCREENINGS that could save your life.
Some services are generally not considered preventive if you get them as part of a visit to diagnose, monitor, or treat an illness or injury. Please be aware that you will be responsible for the cost of any non-preventive care services you receive at your preventive care exam based on your plan design.
Learn more about preventive care at banneraetna.com or aetna.com.
Virtual Care
You have access to virtual care through Teladoc. Get the care you need when and wherever you need it. Whether you’re on the go, at home, or at the office, care comes to you in the form of virtual care.
Get care for non-emergency conditions.
Virtual care can connect you to a doctor, without an appointment, from your phone, computer, or tablet. Receive care for common health issues like allergies, asthma, sore throat, fever, headache, rashes, and much more.
Receive mental health support and counseling.
Licensed counselors and psychiatrists can help diagnose, treat, and even prescribe medication when needed for depression and anxiety, substance abuse and panic disorders, PTSD, men and women’s issues, grief and loss, and more.
Talk with a doctor by phone or video, 24/7.
Use virtual care to prioritize your health by getting the care you need when you
need it. Visit teladoc.com/aetna, download the Teladoc mobile app, or call 800-835-2362 (800-TELADOC) to get started.
MinuteClinic
If you are enrolled in an Aetna medical plan, you have access to MinuteClinic—a walk-in clinic located inside select CVS Pharmacy and Target stores. MinuteClinic is the largest provider of retail health care in the U.S. and makes it easy to find care close to home.
MinuteClinic health providers can:
- Diagnose a variety of illnesses
- Provide vaccinations
- Detect injuries
- Write prescriptions
MinuteClinic is open seven days a week, including evenings and weekends. Schedule your appointment ahead of time or walk-in when it is most convenient for you.
For Open Access Aetna Select Plan and Banner/Aetna Plan members, non-preventive services are covered at 100%. For HealthSave Plan members, after you meet your deductible, non-preventive services will be paid at 100%.
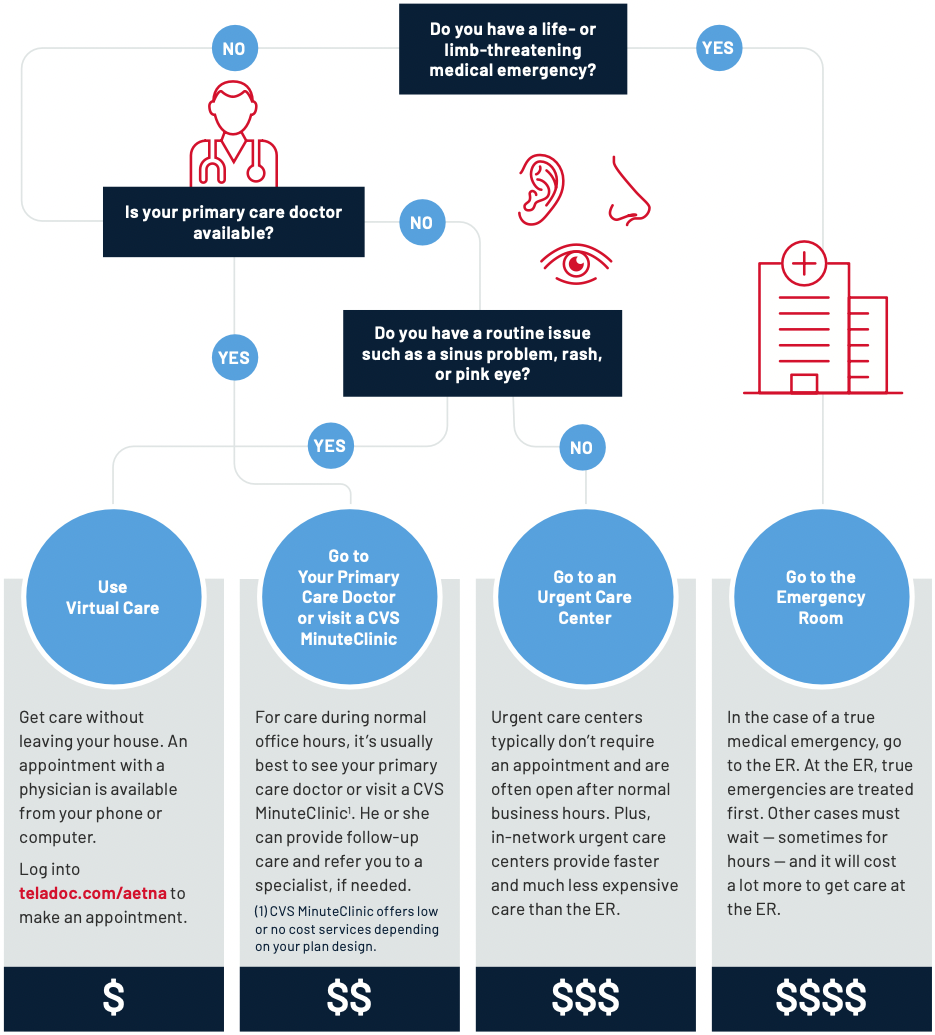
Know Where to Go for Care
Where you go for medical services can make a big difference in how much you pay and how long you wait to see a health care provider. Use the chart below to help you choose where to go for care.
Wellness Resources
FitBucks
If you participate in a Grifols medical plan, you are eligible to receive a $200 reimbursement to get fit. Family members are not eligible for this benefit.
Get cash back for these qualified expenses:
- Gym membership fees (in or out of the GlobalFit network)
- Group exercise classes
- Fitness equipment
- Weight management programs
- Personal training
- Nutritional counseling
- Fitness tracking device
Easy Reimbursement
Sign into aetna.com if you are an Aetna HealthSave or Open Access Aetna Select Plan member, or banneraetna.com if you are a Banner/Aetna member. Then, choose the “Health Programs” tab, and go to “Fitness Reimbursement Program.” You will be directed to the GlobalFit website where you can learn how to get started.
There, you can:
- Find the complete list of eligible expenses
- Submit receipts as often as you wish (up to $200 reimbursement limit)
- Check reimbursement status and more
WellSteps
Grifols provides you with wellness support through the WellSteps portal. WellSteps helps you set wellness goals, participate in simple behavior change tasks, participate in individual and team challenges and campaigns, and engage in health coaching. Track your progress and earn various wellness incentives as well as view the latest health news, videos, and healthy recipes to keep your health on track.
WellSteps is available online or through the mobile app and integrates with several popular fitness devices including Apple, Fitbit, Garmin, and Google. Download the WellSteps app via the App Store or Google Play.
Aetna Tools and Resources
Aetna medical plan members have access to the following resources to help enhance overall health and wellbeing.
Aetna Member Website
The Aetna member website is your online resource for personalized benefits and health information.
When you register you can access the following information on any device:
- In-network providers and facilities
- Benefits and claims status
- Cost estimates for prescriptions and care
Register at aetna.com. Or register at banneraetna.com if you are a Banner/Aetna member.
Aetna One Choice
Whether you’re managing a chronic condition or dealing with other complex health challenges, Aetna nurses can help. If you’re identified for care management, a nurse can work with you to put together a plan, help you understand your benefits offerings, and answer your health-related questions.
Steps to A Healthier Life
This free, online health coaching program lets you choose an area of your health to focus on. And you set the pace, so you can accomplish your health goals in your own time.
- Each program is divided into small steps, so you can benchmark your progress along the way
- Smart, interactive, and fun — Aetna’s online health coaching programs will provide you with strategies for success and
support to meet your goals
Aetna Kidney Support
The Aetna Kidney Support program is designed to help you manage your kidney health and live life to the fullest. The program gives you access to dedicated nurses who can help you get the care you need. As part of Aetna’s total approach to health, it’s available at no cost to you.
Prescription Drug Coverage
Aetna Standard Formulary
A formulary is a list of drugs covered under your plan with details about the type of coverage. Both medical plans utilize the Aetna Standard Formulary. There are certain medications that are not covered under the plans. Log into aetna.com to review the Aetna Standard Formulary.
Aetna Managed Pharmacy Network
The Aetna medical plans utilize the Aetna Managed Pharmacy Network. Locate an in-network pharmacy at aetna.com.
Maintenance Choice
After two retail fills of a maintenance medication, you will be required to fill a 90-day supply of your maintenance drug through Aetna Rx Home Delivery or at a CVS Pharmacy. Your doctor will need to write your prescription for a 90-day supply. Call the toll- free number on your Aetna member ID card for help getting started with 90-day supplies.
Pharmacy Advisor Counseling
The Pharmacy Advisor Counseling program provides face-to-face and telephone counseling to better support members with chronic conditions. These conditions include diabetes, hypertension, asthma, depression, osteoporosis, breast cancer and more.
Prior Authorization
Select Therapeutic Classes of medications will require a Prior Authorization. Precertification is one way that Aetna can help you and your doctor find safe, appropriate drugs and keep costs down. Precertification means that you or your doctor need to get approval from the plan before certain drugs will be covered. If your medication requires a Prior Authorization, your provider will be able to work directly with Aetna to obtain.
24-Hour Nurse Line
Aetna members have access to the 24/7 nurse advice line. These nurses can advise you on care at home, or help determine if you should seek urgent or emergency care. They can also assist in finding nearby facilities and scheduling appointments.
Call the phone number listed on the back of your medical plan ID card.
Enhanced Clinical Review
Medical tests and procedures typically require prior approval before they can be performed. Aetna’s Enhanced Clinical Review Program uses medical specialists and diagnostic tools to review the doctor’s request.
An efficient process delivers the approval in four steps:
- Prescribe: Your doctor orders a test or procedure to diagnose or treat your condition.
- Submit: The doctor’s office submits the request for clinical review.
- Review: Aetna uses a separate independent company, eviCore, to perform the review. eviCore reviews the request using national medical standards, applying the expertise of clinical experts and considering the doctor’s area of expertise. The goal is for you to get the highest medical quality with the lowest out-of-pocket expense.
- Approve: In most cases, the request is approved in a few minutes or less. In some cases, a discussion between doctors is necessary for further clarification.
What Tests and Procedures are Reviewed?
The program covers high-tech radiology services such as MRI/MRA, CT/CCTA, PET, nuclear cardiology, diagnostic cardiology, facility based sleep studies, cardiac implantable devices, hip/knee replacements, pain management, and physical medicine.
Resources
DURING OPEN ENROLLMENT (11/7-12/3) YOU HAVE THREE WAYS TO ENROLL:
- Call 833-557-0382 to speak to a professional benefits counselor.
- Schedule an appointment below with a benefits counselor during the enrollment period.
- Enroll for benefits online at employeenavigator.com/benefits/account/login. Look for the Enroll Now! menu item. If you are a new user, register at employeenavigator.com/benefits/account/register
Your Company Identifier is: CreTestSol