Americhem offers three medical insurance plans through Cigna.
PLEASE NOTE! There is no out-of-network coverage under the EPO plan (only in the event of a life- or limb-threatening emergency).
The table below summarizes the benefits of the medical plans. The coinsurance amounts listed reflect the amount you pay. Please refer to the official plan documents for additional information on coverage and exclusions.
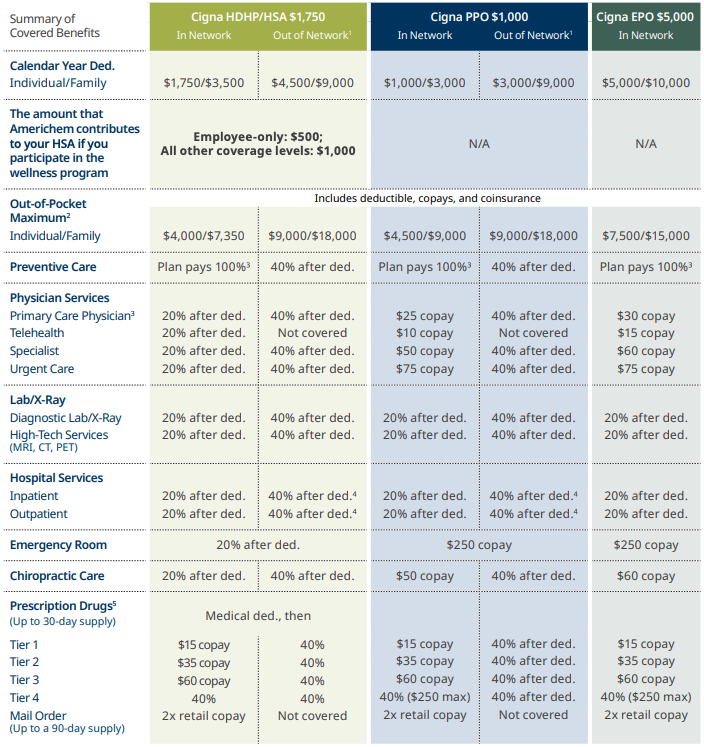
(1) Out-of-network reimbursement based on usual and customary (U&C) charges and average contracted rate (ACR). (2) Plan maximum benefit payment is unlimited. (3) In-network preventive care services are covered at 100%, no deductible or copay applies. (4) Preauthorization required. Failure to do so results in a benefit reduction of $750 with Cigna. (5) For the Cigna HDHP/HSA $1,750 Plan, the deductible doesn't apply for preventive medications.
Resources
WELLNESS PROGRAM INCENTIVES
If you completed the MotivateMe requirements in 2023, you will receive $500 for employee-only coverage or $1,000 for all other coverage tiers.
If you enroll in the Cigna HDHP/HSA $1,750 plan, you will receive this amount via a per pay period incentive deposited into your HSA.
If you enroll in the Cigna PPO $1,000 or the Cigna EPO $5,000, you will receive this amount via a per pay period payroll (cash) incentive.
If you did not complete the MotivateMe requirements in 2024, you will be subject to a $125 surcharge per month in the 2025 plan year. The same applies to your enrolled spouse—if they do not complete the MotivateMe requirements, they will also be subject to a $125 surcharge per month.
To pay less for medical insurance in 2025, participate in the Cigna MotivateMe program.
- Step 1: You and your spouse should complete the Cigna health assessment.
- Step 2: You and your spouse should visit your primary care physician for an annual wellness screen (requires lab work).
Once steps 1 and 2 are complete, you and your spouse may be eligible for additional cash incentives. Be on the lookout for more information.
SPOUSAL SURCHARGE
If your spouse has other medical coverage through their employer and they choose to enroll in an Americhem medical plan, a surcharge will apply. The spouse surcharge is $217 per month. An affidavit will be required and the surcharge will be backdated to January 1, 2024.
TOBACCO SURCHARGE
Employees who certify they are a tobacco user will pay $50 more per month for medical insurance. If you are a current tobacco user and choose to enroll in a tobacco cessation program, you can avoid the tobacco surcharge by successfully completing a cessation program. To enroll in a tobacco cessation program, contact Cigna at 855-246-1873 to learn more about the program and speak with a wellness coach. Or enroll online at mycigna.com with your existing login to access educational materials, support, and begin the selfpaced tobacco cessation program.
If you have any questions about how the program works, please contact Human Resources.
MEDICAL COSTS
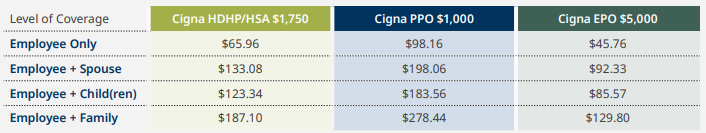
Listed below are the per pay period costs for medical insurance. The amount you pay for coverage is deducted from your paycheck on a pre-tax basis.
ARE YOU COVERING YOUR SPOUSE AND/OR CHILDREN?
If you enroll in the Cigna HDHP/HSA $1,750 plan and choose employee + spouse, employee + child(ren), or family coverage, the individual deductible and out-of-pocket maximum DO NOT apply. The family deductible must be met, either by one individual, or by a combination of family members, before the plan begins to pay. The same rule applies to the out-of-pocket maximum.
PRE-ENROLLMENT RESOURCE—CIGNA ONE GUIDE
Americhem provides you access to Cigna One Guide—a concierge service that helps you make more informed health care decisions. Contact a Guide Representative for help understanding your plan, finding providers, estimating out-of-pocket costs, navigating claims, and more. Start using Cigna One Guide through the app, call 800-244-6224, or visit mycigna.com.
CIGNA MOBILE APP
The myCigna mobile app gives you an easy way to organize and access your important health information. Download it today from the App Store, Google Play, or Amazon for Kindle Fire
Use your myCigna mobile app for the following:
- Find a doctor, dentist, or health care facility.
- View ID cards for the entire family.
- Review deductibles, account balances, and claims.
- Compare costs of medical services.
- Compare prescription drug costs.
- And much more!
MDLIVE
With MDLIVE, you can visit a doctor from your home, office, or on the go. A network of board-certified doctors is available 24/7 by phone or secure video chat to assist with non-emergency medical conditions.
Use MDLIVE for non-emergent health issues:
- Sore throats
- Headaches
- Stomach aches
- Fevers
- Colds and flu
- Allergies
- Shingles
- Bronchitis
- UTIs
- And more
Use MDLIVE for your primary care and preventive care visits:
- Connect with a board-certified primary care provider for routine care.
- Complete your wellness and preventive screenings.
- Receive prescriptions, if needed, that can be sent to your local or home delivery pharmacy.
- Complete blood work, biometrics, and labs at local facilities.
- Acquire referrals to specialists when needed.
Use MDLIVE for virtual dermatology care including:
- Acne
- Eczema
- Dermatitis
- Rashes
- Psoriasis
- Suspicious spots
- Rosacea
- And more
Connect with a licensed physician by visiting mdliveforcigna.com/ or calling 888-726-3171
PREVENTIVE CARE
In-network preventive care is free for medical plan members.
The Americhem medical plans pay 100% of the cost of preventive care when received from a network provider. This means you won’t have to pay anything out of your pocket.

Some services are generally not considered preventive if you get them as part of a visit to diagnose, monitor, or treat an illness or injury. Please be aware that you will be responsible for the cost of any non-preventive care services you receive at your preventive care exam based on your plan design.
Learn more about preventive care at mycigna.com. Select "Medical" and scroll down to "Preventive Care".
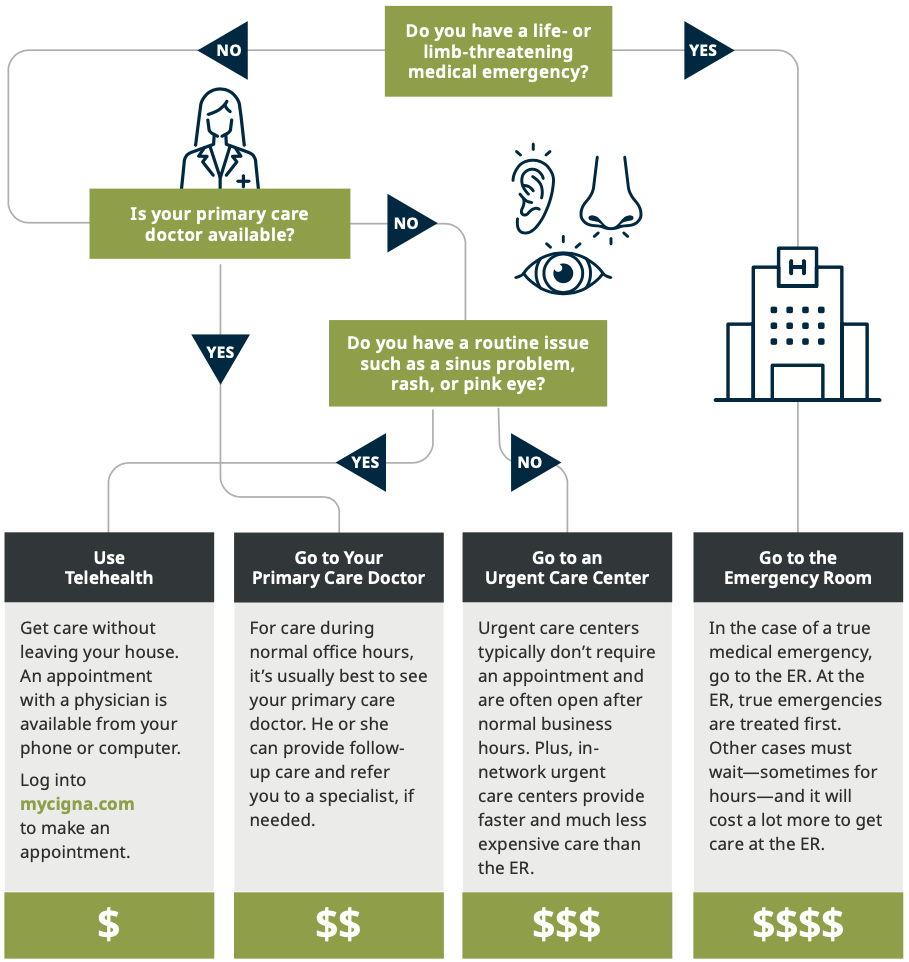
SAVE MONEY ON YOUR HEALTH CARE
PHARMACY PROGRAMS
SPECIALTY MEDICATIONS
Under the Cigna prescription drug plan, you will be able to go to your retail pharmacy for one fill of your specialty medication. Please note, Cigna's pharmacy management program may require prior authorization for specialty and branded medications before they are dispensed. Visit mycigna.com/druglist for a complete list or download the myCigna app and click on "Price a Medication."
Call the number on back of your Cigna ID card, Monday–Friday, 9 a.m.–8 p.m. EST, if you have additional questions.
STEP THERAPY
Step therapy is a prior authorization program. Certain medications in the step therapy program need approval before they’re covered.
Cigna pharmacy management offers step therapy to treat several common medical conditions, including:
- ADD/ADHD
- Allergies
- Asthma
- Bladder problems ◦ Depression
- Heartburn/ulcer
- High blood pressure
- High cholesterol
- Mental health
- Osteoporosis
- Pain (narcotic and non-narcotic)
- Skin conditions
- Sleep disorders
When you fill a prescription for a step therapy medication, Cigna will send you and your doctor a letter explaining what steps you need to take before you refill your medication. This may include trying a generic or lower cost alternative, or asking Cigna for authorization for coverage of your medication. At any time, if your doctor feels a different medication isn’t right for you due to medical reasons, he/she can request authorization for continued coverage of a step therapy medication.
You can find step therapy medications on your prescription drug list at mycigna.com/druglist. If “ST” is listed next to your medication name, then it’s part of the step therapy program.
FORMULARY EXCLUSIONS
A formulary is a list of drugs covered under your plan, with details about the type of coverage. There are certain medications that are not covered under your plan. However, there are preferred alternatives for these conditions that are covered by your plan.
Log into mycigna.com/druglist and select “Value 4 Tier” to review the Value formulary for the medical plan and find out if your prescription is covered.
SAVE ON SPECIALTY
Certain specialty medications are eligible for the SaveOnSP program. If you’re filling an eligible medication, a representative from SaveOnSP will call you to talk about enrolling in the program. If you choose to participate, you’ll pay $0 for your medication. If you choose not to participate in SaveOnSP, you’ll pay a higher cost share when you fill your medication.
SaveonSP can help you save on medications for:
- Multiple Sclerosis
- Oncology
- Hepatitis C
- Rheumatoid Arthritis
- Inflammatory bowel disease
- Psoriasis
PATIENT ASSURANCE PROGRAM
Eligible employees with diabetes will not pay more than $25 for a 30-day supply of insulin using the Patient Assurance Program. Show your Cigna ID card at the pharmacy when you fill one of the covered insulin products listed below. If you’re already using one of the covered insulins, there are no additional steps needed.
- Basaglar
- Humulin
- Humalog
- Levemir
Additional insulin products may be included in the program. If you’re currently taking an insulin that is not included in the program, talk with your doctor about whether taking an insulin covered under the program is right for you. Only you and your doctor can decide what’s best for you.
QUANTITY LIMITS
For some medications, your plan only covers up to a certain amount over a certain length of time. For example, your plan may only cover 30 mg a day for 30 days of a certain medication. These medications have a (QL) next to them on your drug list. Visit mycigna.com/druglist for a complete list.
Medications that typically have quantity limits are often taken in amounts larger than, or for longer than may be appropriate, or are typically misused or abused.
Your plan will only cover a larger amount if your doctor‘s office requests and receives approval from Cigna.
MEMBER PAY DIFFERENCE PROGRAM
Generic medications offer the same strength and active ingredients as the brand-name medications, but often cost much less. Pharmacists automatically substitute generics for brand-name prescriptions unless a doctor specifies a brand is necessary. However, if you still prefer the brand-name medication to the generic, Cigna offers the Member Pay Difference program.
With the Member Pay Difference program, your plan will pay for the cost of the generic medication and put it toward the cost of the brand-name medication. Then you will pay the remaining balance for the brand-name medication. The medical plan will pay no more than the cost of the generic.
MAINTENANCE MEDICATIONS
Maintenance medications are taken regularly, over time, to treat an ongoing health condition.
- A 90-day supply of maintenance medication IS MANDATORY and must be filled at a 90-day network retail pharmacy (CVS, Walmart) or through home delivery Express Scripts.
HOME DELIVERY
Three ways to sign up for home delivery:
- Electronically: For the fastest service, ask your doctor’s office to send your prescription electronically to Express Scripts Home Delivery, NCPDP 2623735.
- By fax: Have your doctor’s office call 888-327-9791 to get a Fax Order form.
- By phone: For current prescriptions, you can transition them to home delivery by calling 800-835-3784.
WELLNESS PROGRAM
Wellness encompasses much more than just eating healthy and exercising. Your mental, emotional, safety, and financial welfare play an important role, too. Americhem’s wellness program is about merging all of those components together.
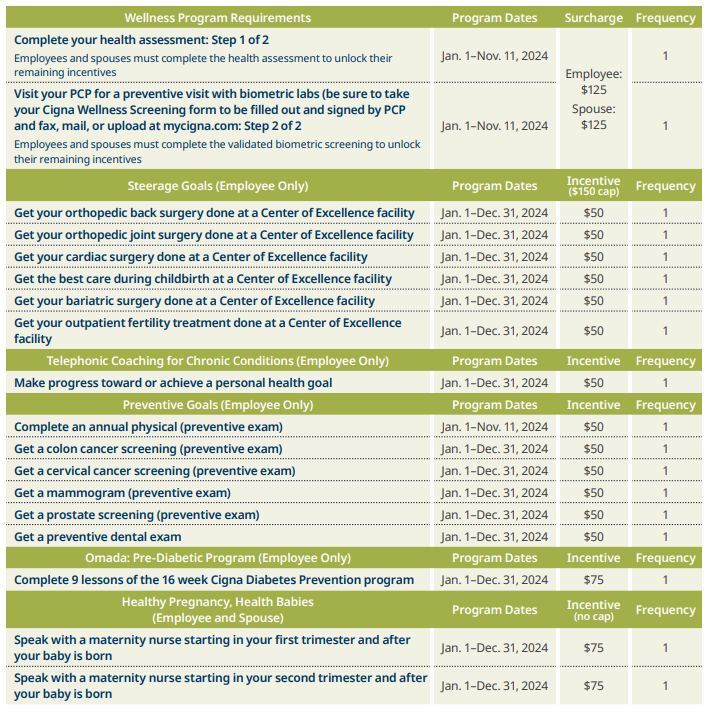
Americhem is committed to helping you achieve your best health. Rewards for participating in the wellness program are available to all employees. You must complete the above goals to earn points. At each point threshold, you will be entered to win one of the associated incentives. If you think you might be unable to meet a standard for a reward under this wellness program, you might qualify for an opportunity to earn the same reward by different means. Contact Human Resources and we will work with you (and, if you wish, with your doctor) to find a wellness program with the same reward that is right for you in light of your health status. Employees hired after August 31, 2024, are not required to complete the wellness program for 2025.
YOUR HEALTH FIRST
As part of your MotivateMe Wellness Program, you have access to personalized health coaching to help you manage a chronic condition.
A dedicated care coach partners with you to help you live a healthier, happier life. You will have access to the following support tools and holistic care solutions:
- Cigna Care Coaching team for one-on-one support, identify barriers, and customize a care plan based on your needs.
- Cross-functional team of clinical experts, including physicians, pharmacists, nurses, certified diabetes educators (CDE), registered dietitians, exercise physiologists, behaviorists, and health educators to connect your care for improved health outcomes.
- Digital tools and online coaching options.
Cigna Care Coaches provide support for the following chronic conditions:
- Heart Disease
- Coronary Artery Disease
- Angina
- Congestive Heart Failure
- Acute Myocardial Infarction
- Peripheral Arterial Disease
- Asthma
- Chronic Obstructive
- Pulmonary Disease (Emphysema and Chronic
Bronchitis) - Diabetes Type 1 and Type 2
- Osteoarthritis
- Metabolic Syndrome/Weight Complications
- Low Back Pain
- Anxiety
- Bipolar Disorder
- Depression
If you qualify, a Cigna Care Coach will reach out to you.
CENTERS OF EXCELLENCE
Going to the hospital can be stressful. Choosing one shouldn’t be. Cigna's Centers of Excellence have identified and ranked top-performing hospitals for 18 common inpatient conditions and procedures, like heart conditions, hip replacements, and surgeries to help you make your own decision.
Cigna has rated these Centers of Excellence above other in-network hospitals when it comes to health outcomes and savings for you for certain procedures or conditions.
Cigna reviews third-party data to compare hospitals’ cost and health outcomes for each of the 18 conditions and procedures factoring in patient experience and cost. Based on all of this fact-finding, a hospital can get up to three stars for health outcomes and up to three stars for cost. If a hospital earns a total of five or six stars for any of the reviewed conditions and procedures, they’re rated as a Center of Excellence for that condition or procedure.
WHY CHOOSE A CENTER OF EXCELLENCE?
Compared to other in-network hospitals, Center of Excellence hospitals have earned a top-rating for health outcomes and can save you money on your health care procedures.
FIND A HOSPITAL
To find Center of Excellence hospitals, go to mycigna.com and select “Find a Doctor or Facility.” Once you’ve accessed the directory, look for the Center of Excellence symbol.
Open Enrollment Has Ended. If You Are A New Hire, Follow The Instructions Below To Enroll:
To enroll in benefits, log into workforcenow.adp.com/public/index.htm . Once logged into the portal, you will be automatically directed to the new hire enrollment wizard. You must complete the enrollment process regardless of whether you are electing or waiving coverage. Coverage begins and ends based on the plan rules.